ERCP Procedure
What is an ERCP?
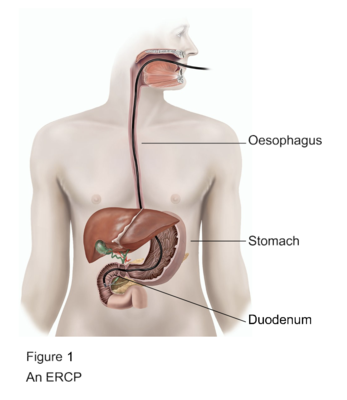
An ERCP (endoscopic retrograde cholangio-pancreatogram) is a procedure to look for any problems in your bile duct or pancreatic duct using a flexible telescope (see figure 1).
Your doctor has recommended an ERCP. However, it is your decision to go ahead with the procedure or not.
This document will give you information about the benefits and risks to help you to make an informed decision. If you have any questions that this document does not answer, ask your doctor or the healthcare team.
Please view our ERCP information sheet
What are the benefits of an ERCP?
Your doctor is concerned that you may have a problem in your bile duct or pancreatic duct. Gallstones in your bile duct or a narrowing of your bile duct are common problems, both of which can cause jaundice (your eyes and skin turning yellow). If the endoscopist (the person doing the ERCP) finds a problem, they may be able to treat it during the procedure.
Are there any alternatives to an ERCP?
There are other ways of looking at your bile duct such as a scan called an MRCP, or a technique called endoscopic ultrasound. These other investigations have fewer complications but cannot be used to treat a problem, which an ERCP is often able to do. You may already have had one of these tests.
If you have a problem in your bile duct, an operation may be an alternative to an ERCP.
What will happen if I decide not to have an ERCP?
Your doctor may not be able to confirm what the problem is. If you decide not to have an ERCP, you should discuss this carefully with your doctor.
What does the procedure involve?
Before the procedure
If you are female, the healthcare team may ask you to have a pregnancy test. They need to know if you are pregnant because x-rays are harmful to unborn babies. Sometimes the test does not show an early-stage pregnancy so let the healthcare team know if you could be pregnant.
If you take warfarin, clopidogrel or other blood-thinning medication, let the endoscopist know at least 7 days before the procedure.
If you have diabetes and take medication containing metformin, let the healthcare team know as soon as possible. You may need to stop taking it on the day of the procedure and for the next two days. You may need to have a blood test after the procedure before continuing with your medication.
Please view our ERCP information sheet
Do not eat in the 6 hours before the procedure. You may drink small sips of water up to two hours before. This is to make sure your stomach is empty so the endoscopist can have a clear view of your stomach. It will also make the procedure more comfortable. If you have diabetes, you will need special advice depending on the treatment you receive for your diabetes.
The procedure may involve injecting you with medication (Buscopan) to relax your stomach and make the procedure more comfortable. Buscopan can affect the pressure in your eyes, so let your doctor know if you have glaucoma.
The healthcare team will carry out a number of checks to make sure you have the procedure you came in for. You can help by confirming to the endoscopist and the healthcare team your name and the procedure you are having.
The healthcare team will ask you to sign the consent form once you have read this document and they have answered your questions.
You may be given antibiotics through a small needle in your arm or the back of your hand.
In the endoscopy room
An ERCP usually takes 30 to 45 minutes.
The endoscopist will give you a sedative to help you to relax. They will give it to you through a small needle in your arm or the back of your hand.
Once you have removed any false teeth or plates, they will usually spray your throat with some local anaesthetic and ask you to swallow it. This can taste unpleasant.
The endoscopist will ask you to lie face down or on your left side and will place a plastic mouthpiece in your mouth.
The healthcare team will monitor your oxygen levels and heart rate using a finger or toe clip. If you need oxygen, they will give it to you through a mask or small tube in your nostrils.
If at any time you want the procedure to stop, raise your hand. The endoscopist will end the procedure as soon as it is safe to do so.
The endoscopist will place a flexible telescope (endoscope) into the back of your throat. You may be asked to swallow when the endoscope is in your throat. This will help the endoscope to pass easily into your oesophagus (gullet) and down into your stomach. From here the endoscope will pass into your duodenum.
The endoscope is then positioned to look at the papilla. The papilla is a small circle of muscle that controls what goes through it.
A fine tube is inserted through the endoscope and into your bile duct or pancreatic duct through the papilla (see figure 2).
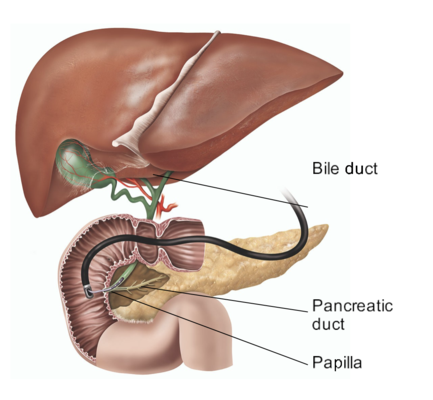
Figure 2 : A tube inserted through the papilla
Dye (colourless contrast fluid) is injected into the ducts and x-rays are taken that show the ducts.
If there are gallstones in your bile duct, they can usually be removed using a sphincterotomy (a cut in the papilla). If the gallstones are large, the endoscopist can insert a stent (tube) in your bile duct to help relieve jaundice. This can also relieve jaundice caused by a narrowing of your bile duct. The endoscopist can carry out these steps using the endoscope and you will not need an operation involving a larger cut.
What complications can happen?
The healthcare team will try to make the procedure as safe as possible but complications can happen. Some of these can be serious and can even cause death (risk: 4 in 1,000). The possible complications of an ERCP are listed below. Any numbers which relate to risk are from studies of people who have had this procedure. Your doctor may be able to tell you if the risk of a complication is higher or lower for you.
- Blurred vision, if you are given a Buscopan injection. This usually gets better after about an hour. Sometimes the injection can also affect the pressure inside your eye. This is more likely if you have a rare type of glaucoma. If your eye becomes red and painful, and your vision becomes blurred, let your doctor know straightaway.
• Allergic reaction to the equipment, materials, medication or dye. This usually causes a skin rash which settles with time. Sometimes the reaction can be serious (risk: less than 1 in 2,500) or even life-threatening (risk: 1 in 25,000). The healthcare team is trained to detect and treat any reactions that might happen. Let the endoscopist know if you have any allergies or if you have reacted to any medication or tests in the past.
- Damage to teeth or bridgework. A plastic mouthpiece will be placed in your mouth to help protect your teeth. Let the endoscopist know if you have any loose teeth.
- Breathing difficulties or heart irregularities, as a result of reacting to the sedative or inhaling secretions such as saliva. To help prevent this from happening, your oxygen levels will be monitored and a suction device will be used to clear any secretions from your mouth. Rarely, a heart attack (where part of the heart muscle dies) or stroke (loss of brain function resulting from an interruption of the blood supply to your brain) can happen if you have serious medical problems.
- Incomplete procedure caused by a technical difficulty, food or blockage in your upper digestive system, complications during the procedure, or discomfort. Your doctor may recommend another ERCP, a different test or an operation.
- Making a hole in your oesophagus, stomach or duodenum, particularly if a sphincterotomy is performed (risk: 1 in 200). You may need further treatment.
- Bleeding, which usually stops on its own (risk if you have a sphincterotomy: 3 in 100). You may need surgery if the bleeding continues.
- Infection. It is possible to get an infection from the equipment used, or if bacteria enter your blood. The equipment is sterile so the risk is low but let the endoscopist know if you have a heart abnormality or a weak immune system. You may need treatment with antibiotics. Let your doctor know if you get a high temperature or feel unwell.
- Inflammation of your pancreas (pancreatitis), which causes abdominal pain and makes you feel sick (risk: 3 in 100). This usually settles within a few days but can develop into serious pancreatitis.
- Infection within your bile ducts (cholangitis) (risk: less than 1 in 100). You will usually be given further antibiotics to reduce the risk of a serious infection.
You should discuss these possible complications with your doctor if there is anything you do not understand.
How soon will I recover?
In hospital
After the procedure you will be transferred to the recovery area where you can rest.
If you were given a sedative, you will usually recover in about an hour but this depends on how much sedative you were given. Once you are awake enough and able to swallow properly you will be given a drink. You may feel a bit bloated for a few hours but this will pass.
You may be able to go home the same day. However, your doctor may recommend that you stay a little longer. If you were given a sedative and go home the same day, a responsible adult should take you home in a car or taxi and stay with you for at least 12 hours. Be near a telephone in case of an emergency.
Returning to normal activities
Do not drive, operate machinery or do any potentially dangerous activities (this includes cooking) for at least 24 hours and not until you have fully recovered feeling, movement and co-ordination.
You should also not sign legal documents or drink alcohol for at least 24 hours.
You should be able to return to work after about two days unless you are told otherwise.
You may get some abdominal pain over the next one to two days. If this becomes worse and you start to vomit, you develop fever and chills, your jaundice gets worse, you start to feel weak and breathless, or your bowel movements turn black, contact the endoscopy unit or your GP. In an emergency, call an ambulance or go immediately to your nearest Emergency department.
Rydym yn croesawu galwadau ffôn yn Gymraeg, Saesneg a Iaith Arwyddion Prydain (BSL) via SignVideo.
We welcome phone calls in Welsh, English and British Sign Language (BSL) via SignVideo.